What type of colorectal cancer screening options do I have?
Colorectal cancer may not be a topic you want to talk about, although companies like Cologuard have done a really great job of making the uncomfortable subject slightly amusing, and more palatable. Yes, that’s the test where you put your poop in a box and ship it off to a lab. But hey…an early diagnosis could save your life.
Let’s rewind a bit. Poop-in-a-box is one of many screening options. It may be right for you, it may not. In the following paragraphs, we will list out a few of the screening options that exist. It’s your job to follow through and get screened for colorectal cancer.
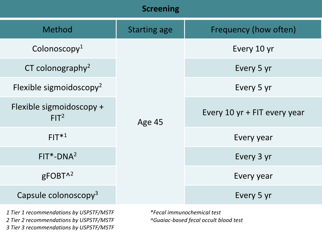
This table lists some of the colorectal cancer screening methods available. The American Cancer Society and the United States Preventative Services Task Force recommend screening begin at age 451. The US Multi-Society Task Force on Colorectal Cancer2 tiered recommendations are based on performance, cost, and practical considerations.
Above all, a colonoscopy is always the recommended test of choice, however the other screening options are not listed in sequential order of importance, but rather are clustered according to endoscopy versus stool-centric tests.
Option #1: Colonoscopy
How often should you have one: Every 10 years
This is the gold standard in colorectal cancer screening. A colonoscopy is the procedure where a long tube with a small camera attached creeps along the inside of your large intestine to examine if there is anything out of the ordinary. While you may blush or cringe at the thought of the procedure, it can be life-saving. And, endoscopists perform this procedure daily…so even though you might be uncomfortable, your healthcare providers aren’t. During this procedure, the endoscopist (the doctor who controls the camera) looks for abnormalities. The inside of a normal colon should look pink and pretty smooth. If the endoscopist sees something “sticking out” (s)he will remove it. It is a growth or a polyp. Having a polyp is not uncommon; about 40% of adults will have a polyp found during a colonoscopy. The majority of polyps are benign or pre-cancerous and a very small percentage are cancerous.
You have to “prep” for this procedure. You will drink a laxative that will flush everything out of your intestinal tract. It is critically important to follow instructions on this step! If you don’t, you risk messing the whole procedure up; the doctor won’t be able to see clearly, the doctor may miss something, and you will likely have to repeat the colonoscopy.
Most adults have some kind of sedation for the procedure, but it is not necessary. Typically, there may be discomfort and cramping, but not really pain. It’s your choice if you would like to be sedated or not.
There are a few risks associated with colonoscopies. You may have an adverse reaction to the sedative (but you can opt out of the sedative). There may be some bleeding if a biopsy was taken. There is a small risk of tearing (perforation) the wall of your large intestine. This last risk is a rare event (less than 1 in 1000 cases) that is more common in older adults (over 75), and in adults with comorbidities, like heart disease or those on blood thinners.
Option #2: Sigmoidoscopy
How often should you have one: Every 5 years
This is similar to a colonoscopy, except that it doesn’t look at the whole colon, it will only look at part of the large intestine. The method may be a bit faster, but it still involves a restricted diet and laxative preparation to clear out your bowel/colon. This option is not advisable for older females or African Americans who are more likely to have colon cancer on the right (proximal) side of the colon—as sigmoidoscopy is unable to evaluate that side of the colon.
Option #3: CT Colonography
How often should you have one: Every 5 years
Instead of having a tube with a camera look at the inside of your large intestine, pictures will be taken using a CT scan (about 6mSv dose of radiation—equal to what you would get naturally over about 2 years). You still have to prep by clearing out your bowel/colon. And if you were thinking you might avoid having a tube up your bum, sorry. To be able to take a good picture, your doctor will place a small tube inside to fill your colon with air. Because you are getting a picture taken of your abdomen and pelvic area, your doctor may see other abnormalities in your kidney, liver, or pancreas that may lead to additional testing. And, finally, if your doctor does see an abnormality in your colon, you will have to have a follow-up colonoscopy.
Option #4: Fecal Occult Blood Test (FOBT)
How often should you have one: Every year
This test looks for blood hidden in your poop. (We’ll use the grown-up word from here on out: stool.) Yes, for this you do need to have a sample of your stool collected and sent to a lab. Why would you have blood in your stool, and what might that mean? If you have a polyp or some abnormal growth in your colon or rectum, there will be blood vessels within that growth. Often times, these blood vessels can be damaged as your digested food passes through you, and a small amount of blood (most often not visible to the naked eye) will be present in your stool.
Side note: You may have previously heard of gFOBT. The “g” in gFOBT stands for guaiac fecal occult blood test. This is an older method, which includes some dietary restrictions and multiple stool collections. Recent data has also shown that the newer methods outperform this method.
Option #5: Fecal Immunochemical Test (FIT)
How often should you have one: Every year
This is a newer version of the FOBT, and it is often called iFOBT (or immunochemical fecal occult blood test). The test does not require dietary restrictions in preparation for the test, and it has better sensitivity than gFOBT. Sensitivity is the true positive rate… which means that if you have colorectal cancer, it is better at detecting it compared to gFOBT. But the specificity of the tests is similar. The specificity is calculated by looking at the true negatives, i.e. the test correctly calls a negative result.
If blood is detected in your stool by gFOBT or iFOBT, then a follow-up colonoscopy will likely be recommended.
Option #6: Stool DNA
How often should you have one: every 3 years
Stool DNA tests look for abnormal DNA that are associated with changes in the colon (like precancerous polyps or colon cancer). There is no bowel preparation necessary for this test, and you only need one stool sample. A follow-up colonoscopy is necessary for a positive result. False positive results are more common with this test, meaning that around 1 out of every 10 people will have a positive result, but nothing will be found during a colonoscopy.
Conclusion: You have lots of options! Colonoscopy is by far the best and most comprehensive option. But there are more potential complications.
If you are at higher risk of developing colorectal cancer, some screening options are more favorable than others. You and your healthcare provider can discuss which option might fit best into your colorectal cancer screening plan.
1. US Preventive Services Task Force. Screening for Colorectal Cancer:US Preventive Services Task Force Recommendation Statement.JAMA.2021;325(19):1965–1977. doi:10.1001/jama.2021.6238
2. Rex DK, Boland CR, Dominitz JA, Giardiello FM, Johnson DA, KaltenbachT, Levin TR, Lieberman D, Robertson DJ. Colorectal Cancer Screening: Recommendations for Physicians and Patients from the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2017 Jul;112(7):1016-1030. doi: 10.1038/ajg.2017.174. Epub 2017 Jun 6. PMID: 28555630.